The keratoconus journey, from first diagnosis to stable management, can take several years – sometimes decades.
Step 1. Initial symptoms
One of the first things you’ll notice in the early stage of this disease as your cornea starts to thin and bulge forward, is a deterioration of your vision. Even through your glasses, things don’t seem as crisp as you would like. Having your glasses prescription changed doesn’t help either. Your prescription may change every few months and the amount of astigmatism will increase.
What does this mean for you? Difficulty with seeing clearly, especially small detail. Driving at night can become very difficult. Your optometrist may investigate what’s going on with your cornea with some additional tests. Or they may refer you to a keratoconus expert. A third option is that they may miss it completely (it only affects 1 on 2000 Australians) and you are left wondering why your vision has deteriorated. You may see several practitioners before finally arriving at a diagnosis.
Step 2. Diagnosis
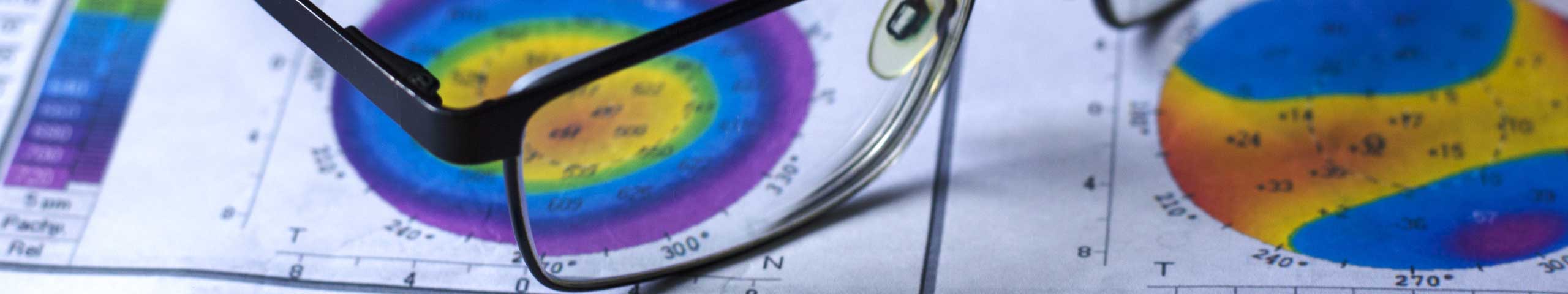
A formal diagnosis is often made by your optometrist. Subtle forms of the disease may need to be diagnosed by a highly experienced keratoconus practitioner – either an ophthalmologist or an optometrist who dedicates their practice to the management this disease. The classic diagnostic tests for this eye disease are:
- Topography, a shape map of your cornea (the front surface of your eye)
- Pachymetry, which measures the thickness of your cornea
Step 3. Discussion and support
One of the problems with diagnosis in many cases of keratoconus is the misinformation that goes with it. Patients are often simply told that they have a progressive eye disease. In the worst scenarios they are told it will eventually lead to a corneal transplant to avoid blindness. This is simply not true for any patient who gets early and appropriate treatment.
Comfortable, healthy contact lens wear can be achieved in the vast majority of cases of this eye disease. But it is important to see someone who knows what they are doing. A surgeon will advise you about the surgical options they provide. They are not contact lens experts. After diagnosis and discussion, you should have a thorough explanation of the disease and its implications for your lifestyle.
Step 4. Management
Glasses may be appropriate, but are often inaccurately measured. This can result in suboptimal vision which pushes you unnecessarily into more aggressive options. An optometrist with expertise in this field will be able to measure you for the best possible pair of glasses. But for most people, they won’t be enough.
Hard (RGP) contact lenses are the mainstay of keratoconus management. They must, however, be fitted by an expert. Inexperienced practitioners with limited lens fitting sets available may achieve good vision BUT with a flat fitting contact lens that can rub the fragile centre of the cornea causing scarring.
If hard contact lenses can’t achieve clear, comfortable vision, there are other options. Specialist lens designs such as hybrid and scleral contact lenses are more expensive and harder to fit, but cater to even the most sensitive eyes.
Step 5. Cross-linking
The majority of people are diagnosed during the progressive stage of keratoconus – in the teens and 20s. During this time, it is possible to have a surgical procedure called Corneal Collagen Cross Linking, which halts the disease in its tracks and prevents further progression.
Step 6. Corneal transplant
While this surgery is rarely required for successfully managed disease, it is sometimes the only option. Eyes that develop the disease in early puberty or cases that have been misdiagnosed or missed for years, can progress to a very severe level of disease. A graft may literally be vision-saving for these people.
It is vital to understand that a graft is a last resort procedure. It is essentially an organ transplant, with all the risks or rejection and failure that with that. Corneal grafts typically last 15 years or so the first time. You can have another graft, but it is only likely to last half as long as the first.
The older you are when you have your first graft, the better. It doesn’t necessarily get you out of contact lenses either. Many people still need contact lenses even after graft surgery.