Retinal Vein Occlusion (RVO) is a vascular disorder where a vein in the retina is obstructed by a clot. It is a painless condition causing vision loss, and is often associated with diabetes, high blood pressure, cholesterol and smoking.
The retina is a very important part of the eye. It is located at the back of the eye and is responsible for capturing pictures of our surroundings and converting them to electrical signals which are transmitted to the visual cortex (vision processing centre) of the brain via the optic nerve. As you can imagine the eye is an extremely complex and “living” video camera.
What is retinal vein occlusion (RVO)?
The retina is supplied with blood though the central retinal artery, which then branches into blood vessels (branch retinal arteries) across the retina. The blood leaves the eye via the branch retinal veins and exits via the central retinal vein. Any blockages to the retinal blood vessels can have disastrous consequences for vision, as the affected part of the retina is starved of oxygen. If the blockage occurs at the optic nerve, it is called central retinal vein occlusion (CRVO). If it occurs at a branch of the retinal veins, it is called branch retinal vein occlusion (BRVO). Branch retinal vein occlusion is 2-3 times more common than central retinal vein occlusion. Blockages to the retinal arteries prevent blood from entering the eye, whereas blockages to the veins prevent blood from leaving the eye. Pressure builds up inside the vessels and widespread bleeding from the veins occurs.
What causes retinal vein occlusion?
Retinal vein occlusion is caused by a blockage in one of the vessels. The vessel walls can become narrowed over time due to fatty deposits (plaque) and it only takes a small blood clot (thrombus) to block the vessel. If the retina is starved of oxygen (ischemic retinal vein occlusion) this can result in a very poor prognosis. The condition is less critical if there are nearby vessels (collaterals) to supply blood to the retina. This is called non-ischemic retinal vein occlusion and has a much better outcome.
What happens in ischemic retinal vein occlusion?
Retinal ischemia causes the eye to quickly build new blood vessels in a process called neovascularisation. This can occur on the retina – particularly around the central, critical part of the retina called the macula. The problem with these blood vessels is that they are faulty, leaky vessels and result in fluid leaking into the retina which can cause permanent vision loss. New vessels can also grow on the iris, the coloured part of your eye, and can block up the eye’s fluid drainage system, causing pressure to build up in the eye and vision loss or blindness through glaucoma.
What happens in non-ischemic retinal vein occlusion?
If there is adequate blood supply to provide oxygen to the retina, RVO causes far less problems. Luckily 75-80% of patients present with this form.
How is RVO diagnosed?
- Retinal vein occlusion is diagnosed by a sudden, painless loss of vision. In non-ischemic RVO, the symptoms are more subtle and intermittent and vision loss is typically mild-to-moderate. In ischemic RVO the symptoms are more marked, with sudden, severe loss of vision and pain may also be present. Usually only one eye is affected but about one in ten cases of RVO is bilateral. If your optometrist suspects RVO, they will refer you urgently to an ophthalmologist.
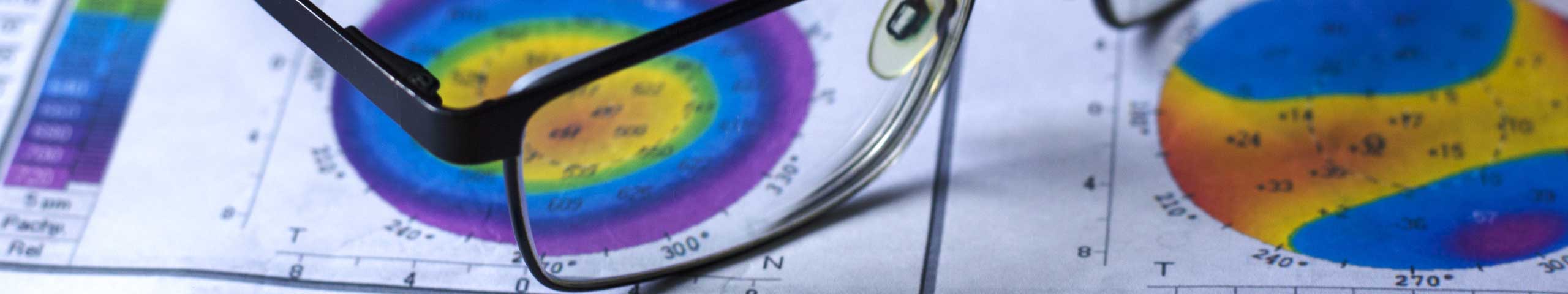
- Your eye specialist will take a detailed medical history including details of when the symptoms began. They will examine your vision, to determine what loss has occurred. They will examine the back of your eyes to look for the widespread haemorrhages that are the classic appearance of RVO. Your intraocular pressure will be measured and your peripheral vision is usually evaluated. Your specialist will also rule out several other retinal diseases that can present with a similar appearance to RVO. A blood test may be ordered and a special dye may be injected into your blood stream to more clearly show the path of blood in your retina. This is called a fluorescein angiography.
What are the risk factors for RVO?
Age
- Patients who develop RVO are often over 65 years of age.
Cardiovascular disease
- 60-70% of RVO patients have high blood pressure
- High cholesterol, diabetes, obesity, smoking and lack of exercise are other risk factors for cardiovascular disease and RVO
- Prevention of RVO is best approached by addressing the risk factors for cardiovascular disease – stopping smoking, losing weight if obese, controlling high blood pressure and diabetes and keeping fit will all assist in prevention of cardiovascular disease and RVO
Other factors
- Blood clotting problems increase risk of RVO
- Raised intraocular pressure (which can lead to glaucoma) is also a risk factor for RVO
What are the symptoms of RVO?
- RVO usually presents with a sudden loss of vision in one eye. Patients often describe it as having a blind spot in one eye. Vision loss may be mild to very severe. Is some mild cases there may be no symptoms.
- RVO is usually painless – especially if the occlusion has recently occurred. Pain may be present at a later stage if there are complications, such as a build of pressure in the eye caused by the formation of faulty new blood vessels blocking the eye’s fluid drainage system.
How is RVO treated?
- There is no way to remove the blockage, although it does resolve spontaneously in some cases.
- Treatment is aimed at managing the complications of bleeding, inflammation and neovascularisation.
- A slow release steroid implant may be placed inside the eye or an anti-inflammatory injection to the eye may be given to reduce inflammation.
- A relatively new treatment, which has only been available for less than ten years, is the injection of a special type of drug (e.g. Lucentis, Eylea) into the eye, which results in clearing up bleeding and can prevent the formation of new blood vessels.
- Management of RVO focuses on prevention of further occurrence in the other eye and thorough assessment of the general health of the patient and treatment of underlying disease.
What is the outlook for RVO?
- Occasionally, RVO may spontaneously resolve, resulting in little or no long-term effect. More commonly, however, retinal vein occlusion results in some residual visual loss. Depending on the site and severity of the occlusion, this can vary widely.
- Early diagnosis and treatment can help reduce complications and improve the outcome, but in the case of severe vein occlusions, permanent vision loss to the eye may result, even if treated early.
- In about 15-20% of cases, RVO recurs (in the same eye or the other eye) within 5 years, so it is imperative to comply with any lifestyle changes and medical treatment that is recommended.
- From a laypersons perspective it is very difficult to determine if any vision disturbance is a specific condition like retinal vein occlusion. The best approach is to visit your optometrist regularly (every year after the age of 60 and as recommended before that).
- If you do notice an unusual vision disturbance, make sure you are proactive and visit your optometrist immediately.
At The Eye Practice we prioritise your general and eye health. If you are concerned about retinal vein occlusion, call us on (02) 92901899 or make an appointment online today and let us put your mind at rest.