Recurrent Corneal Erosion Syndrome (also known as RCES or RCE) is a chronic, relapsing eye condition where the layer of cells on the front surface of the eye repeatedly comes away from the underlying layer resulting in pain, a red eye and other symptoms. Most commonly, this is triggered by the eyelids adhering to the front surface (or cornea) of the eye during sleep. As the eyelids open during waking, sharp pain is experienced and this can persist throughout the day, ranging from uncomfortable to extremely debilitating.
Symptoms
This condition is associated with significant discomfort including:
- pain, (especially on waking) ranging from mild to extremely debilitating
- epiphora (or watering)
- red eyes
- photophobia (or light sensitivity)
- blurred / fluctuating vision
- corneal infections
At its worst, it is almost impossible to keep the eyes open.
Causes of Recurrent Corneal Erosion
Trauma
An injury to the cornea is one of the most common triggers. This is most often a scratch from a baby’s fingernail or a piece of vegetation such as a tree branch or leaf, or even a paper cut. The corneal epithelium is ruptured, but so is the basement membrane it anchors to. This makes it difficult to heal. Although the epithelium regrows quickly, the basement membrane needs 8-12 weeks to repair. During this time, the epithelium can’t attach properly and can easily be sloughed off again by something as gentle as eye movement or opening the eyes on waking.
RCES usually manifests itself several days after sustaining the injury to your eye, but it can appear months later, when you may have forgotten all about the original trauma.
Epithelial Basement Membrane Dystrophy
This disorder, also known as Cogan’s Dystrophy, EBMD or Map-dot-fingerprint dystrophy, is another common cause of RCES. This is where the corneal epithelium is loosely attached to the basement membrane in both eyes, leading to frequent corneal erosions.
A close examination of the eyes reveals weak areas of your cornea that resemble the outlines of maps or fingerprints. If you also have dry eyes, this disease is more likely to flare up and cause symptoms like RCES. This condition is most common between the ages of 40 and 70 and tends to flare up for a few years and then settle down again.
Dry eyes
Chronic
dry eye syndrome can lead to recurrent cornea erosions. If the tear film is inadequate and the corneal epithelium becomes inflamed, the eyelids can adhere to the eye during sleep.
During REM sleep when the eyes are known to oscillate or on awakening the stuck eyelids can cause a subtle or severe erosion, which can be extremely painful.
No time to read the full article? Download our FREE Dry Eye eBook here and learn more about how to manage this condition.
Contact-lens wear
The micro-abrasions from regular contact lens wear can be enough to lead to RCES, especially if the lenses are worn for long periods and you suffer from dry eye.
Rubbing the eyes while contact lenses are worn can lead to microscopic tears in the epithelium and eventually lead to erosions.
Eye surgery
Cataract and refractive surgery can (occasionally) disrupt the attachment of the corneal epithelium and lead to RCES.
Management and treatment options
Your therapeutically-qualified optometrist can provide a range of treatment option for this condition. For the more aggressive treatment options if the condition persists, you will be referred to an ophthalmic surgeon, who can perform therapeutic surgery if necessary. Luckily surgical intervention is not often required.
If you do sustain a traumatic injury to your eye, take it seriously. This is often something that will go on to become a chronic problem.
What follows is a list of strategies from least invasive to most invasive:
Prevention!
Like most things in life, prevention is better than cure. One tip is to always wear your sunglasses when strapping your baby or toddler into their car seat. Injury from a baby’s fingernail is one of the most common causes of trauma-related RCES.
Similarly, when gardening, bushwalking, horse-riding or cross-country running, wear sunglasses to protect the eyes from injury from vegetation.
Blinking
The better the quality of the tear film between the eyelid and the cornea, the less chance of an erosion occurring. Anything you can do to improve your tear function is helpful in managing this disorder. Blink rates have diminished due in part to the digital age of staring at computer screens all day. Blink rehabilitation can help restore a healthy tear film.
Environmental factors
In addition to adequate lubrication, try to avoid excessive airflow while your sleep. Limit the use of aircon or fans, to reduce air circulation. If you must use these devices (due to weather or climate conditions) consider a room humidifier to counter their drying effects.
Hydration
Stay hydrated but avoid fluids before sleep as this can lead to night waking and cause additional symptoms as you open your eyes.
On waking, try not to open the eyes suddenly. Gentle massage or instilling a drop of artificial tears in the corner of your closed eyes can help minimise the adhesion between your eyelids and your eye.
Lubrication at night
Many sufferers of this condition face their biggest challenges at night, when their eyes are more vulnerable to erosions due to depletion of the tear layer.
Lubrication is the mainstay of RCES management. Unpreserved liquid or gel eye drops should be used regularly throughout the day but particularly before sleep.
It can be a matter of trial and error to find what works for you. Some people prefer the added lubrication of an ointment, such as preservative-free VitA Pos (or Chlorsig, which is also unpreserved and has the advantage of giving antibiotic cover to protect from infection).
Others prefer gels or liquid drops. In all cases, you should choose a preservative-free product.
Probiotics / Omega 3
Good quality probiotics have been found to benefit far more than just the gut. In fact, skin health can significantly improve and inflammation can be reduced. Talk to your therapeutically qualified optometrist about which probiotics are most helpful for this condition.
Omega 3 fatty acids from flax oil or fish oil supplements (as well as the foods they naturally occur in) can also help reduce inflammation and restore a healthier tear film.
Manuka honey
Optimel is a product produced from Manuka honey, with anti-inflammatory and anti-bacterial properties. It can help restore an abnormal tear film to better function. This is also hyperosmotic, which allows the epithelium to adhere better to the underlying membrane.
Warm compresses
Just before sleep is a good time to do a warm compress. This is best done with a purpose-designed eye mask such as those made by Bruder. The warm pack should be applied for 15 minutes. This will improve the flow of oily tears if you have meibomian gland dysfunction (MGD) and help lubricate the surface of the eye during sleep.
Physical barrier protection
This may sound obvious but make sure the eyes are closed during sleep. You may need to ask someone living with you to observe your sleeping eyes. Lagophthalmos is a condition where the eyelids do not fully close at night. This exposes a section of the cornea and allows serious dehydration. Over time, this can lead to RCES.
If you suffer from lagophthalmos or a connective tissue disorder called floppy eye lid syndrome, you may need to tape your eyes or wear an eye mask during sleep. Simply covering the eyes reduces evaporative tear loss, keeps in moisture and keeps out moving air from fans etc.
There are many products developed specifically for overnight eye protection (including Tranquileyes goggles and Onyix sleep shield).
Bandage contact lens
Just like a band-aid can help a grazed knee to heal, a contact lens can provide a protective layer between your delicate cornea and your eyelid. This prevent the eyelid from sticking to the front of your eye. Often a soft contact lens in a highly breathable material can allow an eye to heal over 8-12 weeks.
Lenses worn overnight are associated with a higher risk of microbial infections, so this is something that should only be done under the supervision of an eye care specialist. It should be noted however, that RCES itself is associated with a risk of corneal infection due to break in the surface layer of the eye. A supervised bandage contact lens can allow the eye to heal and ultimately lead to a better, safer outcome and a healthier eye.
Prednisolone preservative-free eyedrops
Inflammation on the ocular surface causes swelling of the cornea. This makes it easier for the cells to slough away, leading to further erosions. A powerful anti-inflammatory, used in conjunction with doxycycline or azithromycin (see below) can improve the function of the oily tear glands in the eyelids and improve tear quality.
Oral Doxycycline / Azithromycin
These oral medications are prescribed for weeks to months. They work by changing the constitution of the oily tear film from the inside out.
IPL
Ocular rosacea is sometimes associated with recurrent corneal erosion.
Intense pulsed light (or IPL) can improve dry eye symptoms for patients with ocular rosacea. This in turn can improve symptoms of RCES.
Surgical treatments
Stubborn cases of RCES require surgical intervention. This can literally be life-changing so don’t feel you have to live with your symptoms. Patients have reported levels of distress with RCES to the extent that that have considered having their eye removed to stop the symptoms! A little surgery – where indicated – can be enormously beneficial.
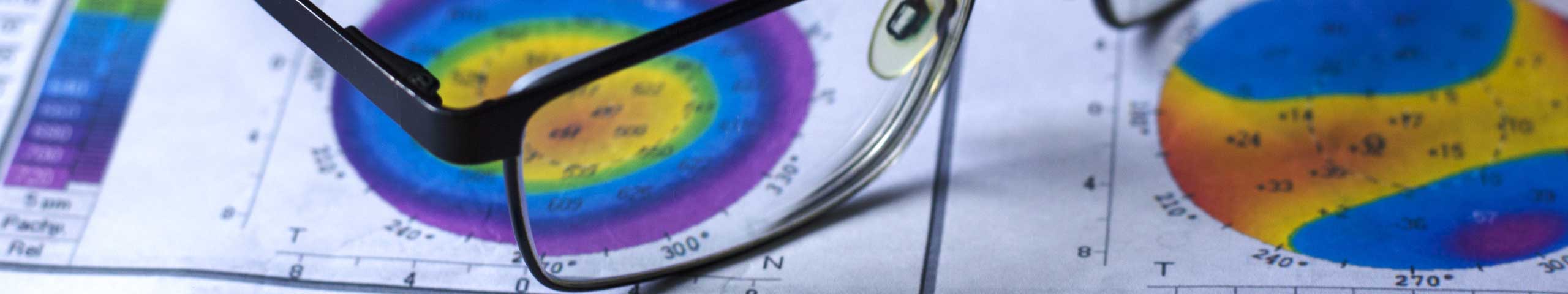
Basement membrane debridement
In this treatment, the surgeon peels away the top layer of cells from the whole cornea, so it can regenerate as one continuous layer. A bandage contact lens is usually worn for the first few days after the procedure until the epithelium is intact.
Stromal puncture
This is performed by an ophthalmologist and involves making a series of tiny pin-pricks in the cornea in the affected area. These allow the epithelium to anchor more tightly as it regrows.
Therapeutic PRK
This is a laser procedure that removes a thin layer of cells from the whole cornea. The idea is a bit like sanding back an uneven surface. It allows the basement membrane and epithelium to regenerate afresh, as a single layer, rather than trying to patch up a small area or irregularity.
This is the ultimate treatment for RCES but also the most invasive and only advised where less invasive strategies have failed.
Recurrent corneal erosion is a seriously debilitating condition with a range of treatment options. You don’t have to live with it. Come and see the experts. Call The Eye Practice on (02) 9290 1899 or make an appointment online today.