While diagnosis of this disease is complicated, the goal of glaucoma treatment is very simple: to avoid nerve damage, preserve visual field and ensure continued quality of life. This involves adequately lowering intraocular pressure (IOP). Achieving this goal, however, can be easier said than done.
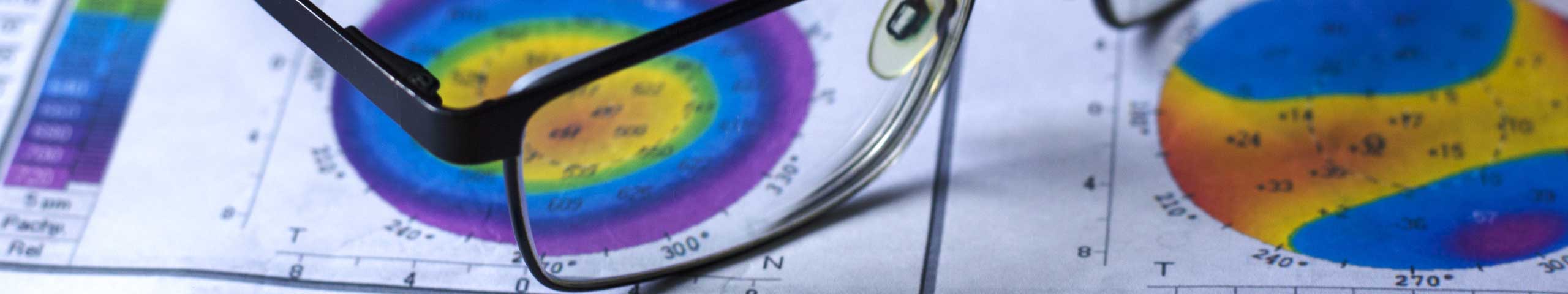
The Advanced Glaucoma Intervention Study (AGIS) studied the eyes of nearly 600 patients with glaucoma over a 14-year period. It clearly showed a direct relationship between IOP and progressive visual field loss – i.e. permanent damage to the retinal nerve fibres that worsens over time.
Specifically, the results of the study showed that patients who consistently maintained their IOP at less than 18mmHg at ALL follow-up visits and had average pressures of 12mmHg, had almost no glaucoma progression over the 14 years of the study.
The study showed that the more the pressure varied at follow-up visits, the higher the incidence of visual field loss over time. This shows how vitally important compliance is in the management of this disease. This means two things; use the eyedrops exactly as prescribed and return for regular follow up.
How do we lower IOP?
Eye drops
IOP-lowering eye drops are the mainstay of glaucoma treatment and there are many different types available.
The most commonly prescribed IOP-lowering drops are the prostaglandin analogues, as they have very few side effects. These drops work by allowing intraocular fluid to exit the eye more easily and include Travatan, Xalatan and Lumigan (which is also available in a preservative-free formula – a huge boon for dry eye patients).
There are a number of other classes of IOP lowering eyedrops which may also be prescribed, (including beta-blockers) depending on your particular type of glaucoma and your medical history.
Sometimes, one drop is not enough to attain the target pressure, and a second drop may be added, or more commonly, a combination drop (Combigan, CoSopt or Simbrinza). You are more likely to consistently use one drop every day than two different drops.
Laser
Some patients find it hard to comply with eyedrops regimens. This may be due to frequent business travel in younger patients, or to dementia in older patients. Selective laser trabeculoplasty (SLT) is another option for increasing the outflow of fluid from the eye. It involves lasering the angle of the eye (between cornea and iris) to open it up. SLT may be required as well as eyedrops, if IOP is not coming down to the desired levels with just one therapy.
What if drops and laser are not enough?
Minimally invasive glaucoma surgery (also called MIGS) refers to the placement of a small stent-like device inside the eye, during an intraocular procedure, most commonly cataract surgery. One of the most commonly used is called the iStent, which bypasses the drainage meshwork of the eye, allowing fluid to drain more easily.
Note: All glaucoma therapy is invasive – whether drops, laser or MIGS devices like iStent. Your specialist will be able to advise you on the least-invasive therapy for your particular circumstances.
Injections / slow-release implants
Phase 3 trials are now underway in Australia to test the effectiveness of sustained-release implants containing the anti-glaucoma medication bimatoprost. These tiny implants are injected inside the eye, where they slowly release the drug. Early results show that the reduction in intraocular pressure is similar to topical medication (eye drops). The advantages of this mode of drug delivery are, firstly, compliance – no need to think about putting in eyedrops – and secondly, reduced red eye.
Can surgery help?
Cataract surgery
This procedure is only ever indicated if you have a clinically significant cataract, but it does have a very beneficial side effect of lowering IOP and improving your glaucoma prognosis. So, if you have glaucoma and then you develop a cataract, having surgery will help address both problems.
Filtering surgery
When less invasive therapies fail, it’s time to bring out the big guns. Glaucoma surgery procedures are not a cure for the disease, but a temporary solution – they buy more time. Trabeculectomy involves surgically removing part of the eye’s trabecular meshwork. This is the filtration mesh that allows fluid to drain out of the eye. If the mesh is too fine, the fluid can’t escape fast enough. Removing a portion allows fluid to leave the eye much more easily to underneath the conjunctiva, where it is absorbed.
Compliance – why bother?
The most important take-home message is this: Most glaucoma-related vision loss comes down to poor compliance. What does that mean? It simply means that in order to achieve the best outcomes, and the least amount of further permanent damage to your eyesight, you do have to follow your eyecare practitioner’s exact instructions regarding eyedrops and return to the practice to monitor your progress.
Many people go blind from this disease through failure to use their drops or to return for follow up.
Remember: if you can keep you IOP around 12mmHg and always below 18mmHg, there is little likelihood of further damage occurring. You will only know this if your optometrist or ophthalmologist can measure it regularly, and adjust your therapy if you are not achieving the required drop in IOP.
A big problem is that, in most cases, glaucoma has no symptoms, whereas putting in drops every day can be a costly inconvenience and literally a pain – as they can sting. However, compared to permanently losing your eyesight, a few eyedrops don’t seem so bad.
Laser Peripheral Iridotomy (LPI or PI)
If you have narrow angles, you are at risk of the angle between your cornea and your iris closing up and preventing any outflow of fluid from your eye. This can happen suddenly in an acute angle-closure attack, or more gradually. Intraocular fluid normally flows through your pupil into the front chamber of your eye, where it drains away at the edges of your cornea. If the pupil becomes blocked, the fluid cannot get out and pressure builds up very quickly, causing damage to the optic nerve. A very effective prevention for this for anyone at risk of angle closure is to have a peripheral iridotomy – which is a small hole created in the iris of your eye. The hole is near the outer edge and is not visible to the naked eye. It allows fluid to bypass the pupil and pass directly to the front chamber of the eye. It is created using a special type of laser and is relatively quick and painless.
Finding your glaucoma therapy confusing? At The Eye Practice, we have the time to explain your disease and your therapy clearly to you. We can even refer you to another glaucoma specialist for a second opinion if you are finding it difficult to comply with your current treatment.
Call us on (02) 9290 1899 or make an appointment online today.